Sufferers
A complete of 36 consecutive sufferers admitted through the interval of September 2018 to December 2019 have been enrolled on this research, encompassing 31 males and 5 ladies aged 22 to 71 (median 39.5 ± 25.75). Thereinto, 13 sufferers underwent preoperative DCE-MRI however not postoperative MRI, 14 sufferers underwent postoperative DCE-MRI and preoperative typical MRI (non-DCE-MRI), and 9 sufferers underwent each preoperative and postoperative DCE-MRI. All sufferers on this research have been affected by idiopathic cryptoglandular anal fistulas, whereas different secondary anal fistulas have been excluded, corresponding to Crohn’s illness, tuberculosis and malignancies.
MRI examination and approach
MRI examinations have been carried out on a 3.0 T MR scanner (Vantage Titan, Canon Medical Programs Company, Japan), utilizing a 16-channel floor coil. Sufferers have been imaged in a head-first supine place with the middle of the magnetic discipline on the pubic symphysis. Previous to the MRI examination, no particular bowel preparation was administrated, and no antispasmodic agent was required as a premedication. Indirect axial and coronal pictures have been obtained by orientation perpendicular and parallel to the anal canal. For all sufferers, all MRI scans are carried out with the identical protocol (Desk 1).
DCE-MRI was carried out utilizing a dynamic three-dimensional T1-weighted quick discipline echo imaging (3D-T1-FFE) with the next sequence parameters: TR = 3.7 ms, TE = 1.3 ms, flip angle = 12 levels, bandwidth = 488.2 Hz/pixel, slice thickness = 4 mm, intersection hole = 0 mm, variety of slices = 26, acquisition matrix = 192 × 192, FOV = 250 mm × 200 mm. Consecutive imaging was composed of 20 repeated scans with a complete scan time of three min 46 s. Ranging from the second repeated scan, the distinction agent (Gadopentetate Dimeglumine Injection, Shanghai Xudong Haipu Pharmaceutical Co., Ltd, China) was administered intravenously at a dose of 0.1 mmol/kg (0.2 ml/kg) of physique weight by way of an 22-gauge intravenous catheter with an automatic injection pump (Optistar Elite, Liebel-Flarsheim Firm LLC, USA). After bolus injection (3 mL/sec) of the distinction agent, a 15 mL saline answer was instantly injected on the similar fee. An Indirect axial T1-weighted quick spin echo (FSE) sequence with fats suppression was carried out in the long run.
Picture evaluation
St James’s College Hospital classification
The St James’s College Hospital classification is a MR imaging-based grading system that may be simply utilized and might precisely assess the connection between major fistula tracks, secondary extensions, abscesses and regular anatomical constructions. The system is split into 5 teams [20]: Grade 1, easy linear intersphincteric fistula; Grade 2, intersphincteric fistula with abscess or secondary monitor; Grade 3, transsphincteric fistula; Grade 4, transsphincteric fistula with abscess or secondary monitor inside the ischiorectal fossa; Grade 5, supralevator and translevator illness.
Normalized sign depth
Primarily based on the quadriceps muscle as a reference organ, the normalized sign depth (NSI) was outlined as a ratio of fistula wall to quadriceps muscle sign on the indirect axis fat-suppressed T2-weighted picture.
Semi-quantitative parameters of DCE-MRI
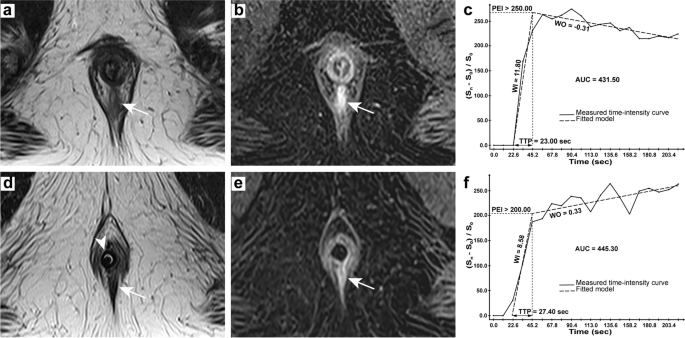
All DCE-MRI semi-quantitative parameters are primarily based on the form and construction of the time-intensity curve (TIC), together with wash-in fee (WI), wash-out fee (WO), time to peak (TTP), peak enhancement depth (PEI), space underneath the curve (AUC), have been calculated on the imaging workstation (Myrian V1.12, Intrasense, France) (Fig. 1). The focus computation technique used to generate parametric maps was set to (({textual content{S}}_n-{textual content{S}}_0)/{textual content{S}}_0) (a relative normalization utilizing the baseline) the MR collection. Areas of curiosity (ROIs) have been positioned on the fistula wall and therapeutic tissue. Three areas with the very best enhancement (often 17–19 occasions in 20 repeated scans) have been measured, and the typical worth was taken as the ultimate worth, with a median of three.84 mm2.
42-year-old man presenting a easy linear intersphincteric fistula. Preoperative MRI: axial T2-weighted picture (a) displaying the lively fistula in hyperintensity (arrow), axial DCE picture (b) displaying early sturdy enhancement of the fistula (arrow) and TIC with parameters (c); Postoperative MRI: axial T2-weighted picture (d) displaying the therapeutic tissue in hypointensity (arrow) and a balloon catheter (arrowhead), axial DCE picture (e) displaying progressive enhancement of the lesion (arrow) and TIC with parameters (f)
Normal of Reference
Medical signs, MRI manifestations, outcomes of anoscopic examination, intraoperative findings in addition to pathological outcomes have been used as diagnostic standards for lively fistula, and the interval between preoperative MRI examination and operation was lower than three days. If there have been no scientific signs through the postoperative MRI reexamination and no recurrence in a scientific follow-up for at the least six months after the reexamination, it was labeled as postoperative therapeutic (granulation) tissue. If there have been scientific signs and suspected residue or recurrence of fistula monitor on MRI pictures, which was later confirmed by surgical procedure and pathology, it was labeled as lively fistula.
Statistical evaluation
Descriptive statistics have been offered as median ± interquartile vary for non-normally distributed steady information and as numbers and percentages for categorical variables. The distinction in classifications of anal fistula between two predefined teams was analyzed utilizing Mann-Whitney check. Spearman’s correlation check was carried out between time intervals and parameters of postoperative MRI reexaminations. The variations in MRI parameters between 4 predefined teams have been quantitatively in contrast utilizing Kruskal-Wallis check, after which receiver working attribute (ROC) curves have been used to judge the diagnostic skill, together with the optimum cutoff, space underneath curve (AUC) with 95% confidence interval (CI), sensitivity, and specificity. ROC curves have been performed with MedCalc 19.2 (MedCalc Software program Ltd, Ostend, Belgium; https://www.medcalc.org), and different statistical analyses have been carried out utilizing SPSS 26.0 (IBM Company, Chicago, USA). A two-tailed p worth of lower than 0.05 is taken into account to point statistical significance.